2024 Senior Healthcare State Report Cards
The American healthcare system can be challenging to navigate and afford for people of any age, but its flaws are especially pertinent to Americans 65 and older. Older people often endure declining health while relying on fixed incomes and Medicare coverage. Rising costs for elderly health care have even led some seniors into financial ruin. Finding affordable, available, and effective healthcare can be critical to maximizing retirement years.
To aid in that search, SeniorLiving.org conducted a detailed analysis of nationwide healthcare conditions for older adults. We documented elderly medical care access, costs, and outcomes nationwide and ranked each state’s performance. We also surveyed 500 Americans aged 65+ regarding the importance of healthcare and specific medical priorities. The results revealed that older Americans may want to rethink the most popular retirement destinations if quality healthcare is a priority.
Read on for a coast-to-coast report card detailing the best and worst states for senior healthcare and a breakdown of regional strengths and weaknesses.
Key Findings:
- Montana and North Dakota earned A+ grades for healthcare quality, while six states (Mississippi, North Carolina, Oklahoma, Delaware, Alabama, and West Virginia) got F grades.
- One of America’s top retirement destinations, Florida, earned a D+ for senior healthcare and outcomes. Arizona, another popular state, earned a B grade.
- Washington earned the top score for healthcare affordability, and West Virginia had the highest expenses.
- Heart disease is the most prevalent medical concern for America’s seniors, and Minnesota boasts the lowest mortality rate for that illness.
- Two-thirds of older Americans say healthcare policies will be “very important” or “extremely important” in determining their presidential vote this November.
Senior Healthcare Grades by State
On average, older adults – who will make up 21 percent of the population by 2030 – devote three weeks per year to doctor’s visits and other health appointments. Such an investment of time among an expanding demographic portends a looming care crisis and highlights the integral role medical attention assumes in everyday senior life.
Below is a report card on every state's overall senior healthcare status. Grades were derived from a composite ranking of each state’s performance across several categories: healthcare accessibility, costs, and outcomes for those aged 65+ (the methodology is detailed below).
Two states (Montana and North Dakota) stood out from the crowd with honors-worthy “A+” scores, with another three states (South Dakota, Minnesota, and California) securing solid “A” marks. Six territories (Mississippi, North Carolina, Oklahoma, Delaware, Alabama, and West Virginia) posted failing scores.
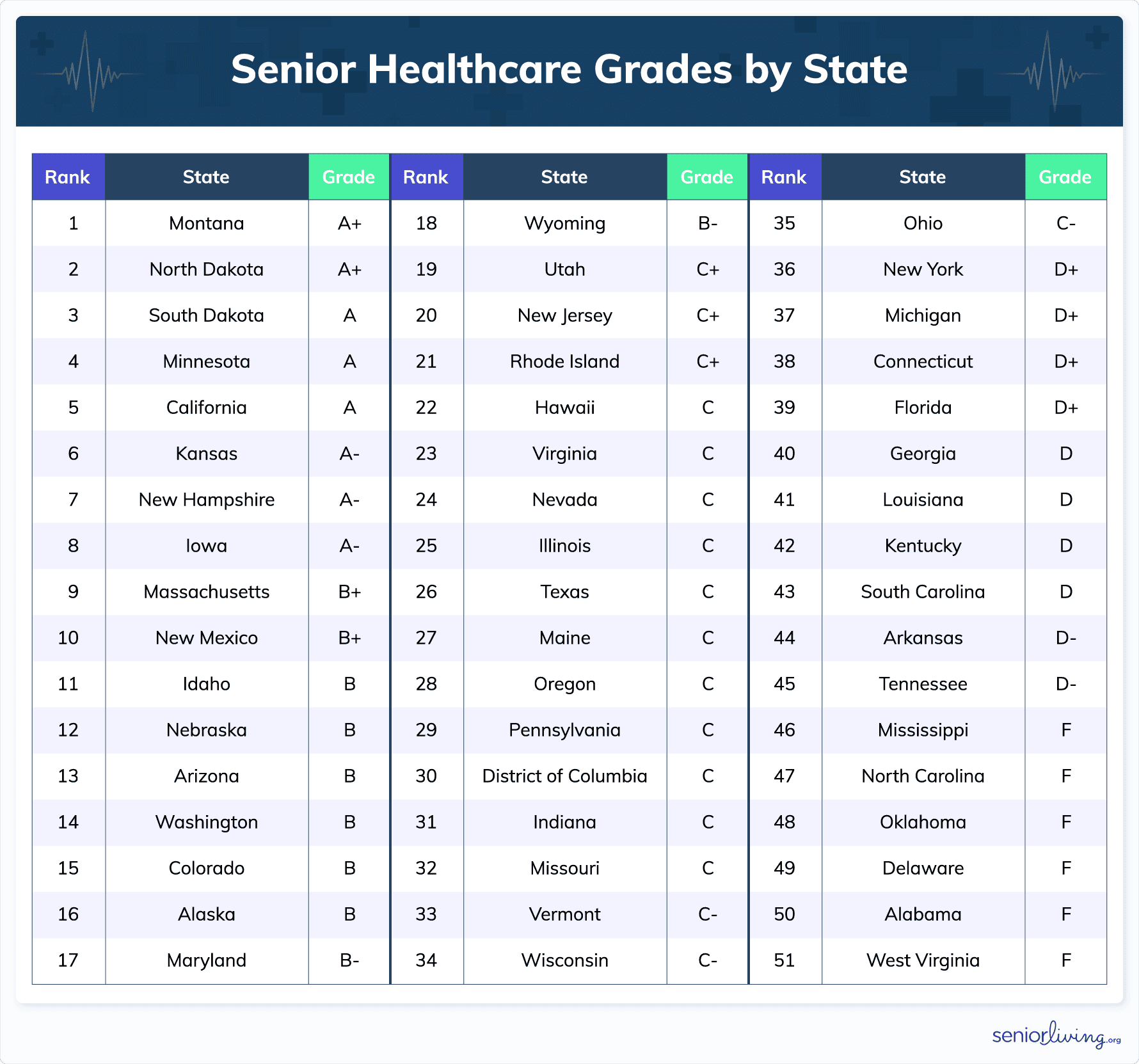 Several Midwestern states topped the ranking. This was due, in part, to the region’s network of renowned hospitals (the Mayo Clinic, Sanford Health, Cleveland Clinic), abundant medical research centers, and device manufacturers (3M, Medtronic) that focus local economies on the sector.
Several Midwestern states topped the ranking. This was due, in part, to the region’s network of renowned hospitals (the Mayo Clinic, Sanford Health, Cleveland Clinic), abundant medical research centers, and device manufacturers (3M, Medtronic) that focus local economies on the sector.
The South fared particularly poorly on the report card. All 12 states with grades of “D” or worse lie in America's South. These results are likely the result of several sociodemographic and economic influences. Obesity is more prevalent in the region, which is one factor fueling higher concentrations of chronic diseases. Poverty is also highest in the South, which can also lead to poor health results and underfunding of medical infrastructure.
Let's look at the five best and worst-graded states for older American healthcare.
The Best States for Senior Healthcare
1. Montana – Overall Grade: A+ (100)
Montana may be known for its badlands, but it is an excellent land for senior healthcare, notching the best overall grade in the nation. The state’s primary strength was its healthcare accessibility for older citizens. With a population of just over 1.1M, its healthcare access score was second among all states – a number aided by the Montana Rural Physician Incentive Program that subsidizes and attracts medical professionals. Montana also had many Medicare hospitals per resident aged 65 or older. Additionally, Montana has been on the leading edge of telehealth initiatives designed to aid a dispersed citizenry comprising the third lowest population density in the country.
The state also ranked 7th for its healthcare cost score, thanks to moderately lower insurance premiums and annual drug costs, which are about 40 percent lower than the national average. A notably low death rate from strokes helped its medical outcomes score, which was 18th best in the country.
2. North Dakota – Overall Grade: A+ (98.3)
The only other state with an A+ rating was Montana’s neighbor, North Dakota. Perhaps not coincidentally, these two top states also border patient-friendly Canada. North Dakota earned its top marks by demonstrating consistency across all categories. It ranked fifth in the country for its high accessibility score, meaning seniors in Fargo needn’t “go far” to find a medical provider. It was ninth for its medical outcome score, driven by markedly low death rates for cancer and nominally lower-than-average mortality rates for strokes.
North Dakota ranked 17th among the states for senior medical costs, aided by insurance premiums 18 percent below the national average and drug costs lower than most. North Dakota’s nursing homes are also known for superior staffing benchmarks.
3. South Dakota – Overall Grade: A (92.9)
Mount Rushmore’s Founding Fathers are smiling about senior health care in South Dakota. The state earned an “A” grade – appropriately, just below that of its northern partner. South Dakota nabbed its exemplary grade by posting the top score for elder care availability. Its abundance of nurse practitioners, Medicare providers, and Medicare hospitals ensures seniors have ample opportunities for medical attention.
It also ranks 20th for medical costs, thanks to annual drug expenses 21 percent below the national average, and has relatively low death rates for strokes and heart disease.
4. Minnesota – Overall Grade: A (92.6)
Home to the world-famous Mayo Clinic and medical device suppliers 3M and Medtronic, Minnesota features 10,000 lakes and the 4th best rating for senior health care. Reasonable medical pricing is Minnesota's strongest selling point. The state ranks second nationally for its healthcare cost score, with annual drug pricing and insurance premiums 27 percent lower than national averages.
Minnesota also features excellent medical outcomes, buoyed by the nation’s lowest death rate from heart disease, along with impressive mortality rates for strokes and cancer. Additionally, Minnesota gets credit for its comforting initiatives for older citizens with medical issues; the state has generous grant programs to help keep seniors in their homes and provides payment and training to family caregivers.
5. California – Overall Grade: A (92.3)
California was ranked just behind Minnesota, meaning the Golden State is an attractive place to live out one’s golden years. With an excellent network of world-class facilities and a holistic CalAIM program, positive outcomes represent California’s calling card. The state ranked sixth in this category, posting mortality rates well below the national averages for cancer, heart disease, and falls. In fact, California was in the top 10 for each of these categories.
Additionally, California supplies excellent access to hospice care and Medicare facilities while keeping expenses slightly below nationwide norms. Like Minnesota, it emphasizes home care through its Programs of All-inclusive Care (CalPACE) initiative.
The Worst States for Senior Healthcare
1. West Virginia – Overall Grade: F (35.3)
With a healthcare system overwhelmed by an opioid crisis, West Virginia has fewer resources to devote to elderly care. That fact, combined with the state’s prevalent behavioral risk factors, poverty rates, and chronic disease, helps to explain why WV is ranked #49 out of 50 for senior medical outcomes. West Virginia also posted the nation’s worst healthcare cost score, as older residents are burdened with high costs for insurance, prescriptions, and out-of-pocket expenses. In fact, the average monthly health insurance premiums were 71 percent higher than the national average.
However, the state has many Medicare providers and hospitals, so older West Virginians may have an easier time accessing affordable care than in other states.
2. Alabama – Overall Grade: F (37.5)
Bad tidings roll across Alabama for older citizens in need of medical assistance: the state is the second worst in the union for seniors seeking healthcare. Alabama has issues with chronic disease and poverty, leading to high hospitalization rates for manageable diseases like diabetes. The state ranked 44th for its medical outcome score and has one of the lowest life expectancies in the nation. In many rural areas, older Alabamians have limited access to healthcare professionals and have the fourth-worst healthcare costs in the country.
3. Delaware – Overall Grade: F (39.1)
Commonly known as the “First State,” Delaware placed nearly last regarding senior healthcare. It's the only state to rank 40th or worse in all three categories used in our grading system: with one being the best, Delaware ranked 44th in healthcare costs, 40th in access, and 41st in outcomes. Drug costs in the state were exceptionally high, 39 percent higher than the national average.
Additionally, the state had the worst stroke death rate in the nation and was as were death rates from cancer and strokes. One unique challenge for Delaware is its rapidly aging population, which is growing older at a rate far faster than the nation, stretching limited resources earmarked for senior care.
4. Oklahoma – Overall Grade: F (40.5)
Those requiring medical attention in Oklahoma should seek it “sooner” rather than later, as the state is one of the worst in the nation for providing senior healthcare. Oklahoma’s greatest challenge is medical outcomes—only Mississippi’s score in this area is worse. Oklahoma has the highest mortality rate for heart disease, the fourth-worst for cancer, and the sixth-worst for death from falls. The state also has higher-than-average out-of-pocket medical expenses and insurance premiums for older citizens.
5. North Carolina – Overall Grade: F (40.6)
North Carolina is the fifth worst state in America for elderly health care, scoring an overall “F” for its services. The Tar Heel State had the worst healthcare access score, given its very limited availability of hospices, Medicare providers, and Medicare hospitals for older residents. It also ranked 37th out of 50 for medical costs, with exceptionally high pharmaceutical prices for seniors. North Carolina’s high death rates from strokes and falls leave it ranked #36 for health outcomes.
State Rankings by Healthcare Category
Our analysis considered myriad factors spanning three broad components of senior healthcare: outcomes, accessibility, and cost. Each of these areas included several subcategories to generate a comprehensive picture. To aid older Americans with specific needs or concerns, here are the best and worst states for each facet of care.
Senior Medical Outcomes
The ultimate measure of any healthcare plan is its efficacy in treating the patient; access and costs become irrelevant if an older patient loses their medical battle. To assess each state’s performance, we considered mortality rates from four afflictions that regularly affect elderly citizens: cancer, heart disease, strokes, and falls. Our survey of citizens 65 and older revealed that they are most concerned about outcomes for heart disease, followed closely by cancer.
The top five states for senior healthcare outcomes, particularly in the treatment of the most important issues, were located predominantly in America’s Northeast, and many of the worst were in the South. Mississippi is the lowest-ranked state for medical outcomes by an uncomfortable margin and had the worst cancer outcomes, in particular.
| States with best outcome scores | States with worst outcome scores |
|---|---|
| New York | Mississippi |
| New Jersey | Oklahoma |
| Hawaii | West Virginia |
| Massachusetts | Tennessee |
| Connecticut | Louisiana |
Healthcare Availability for Seniors
America’s healthcare system already faces a staffing crisis that will worsen as the nation’s population grows older. The availability of medical professionals and facilities is particularly strained in rural areas nationwide. Our accessibility rankings considered the ratio of residents to providers within five categories: physicians, nurse practitioners, hospices, Medicare-certified providers, and Medicare-certified hospitals.
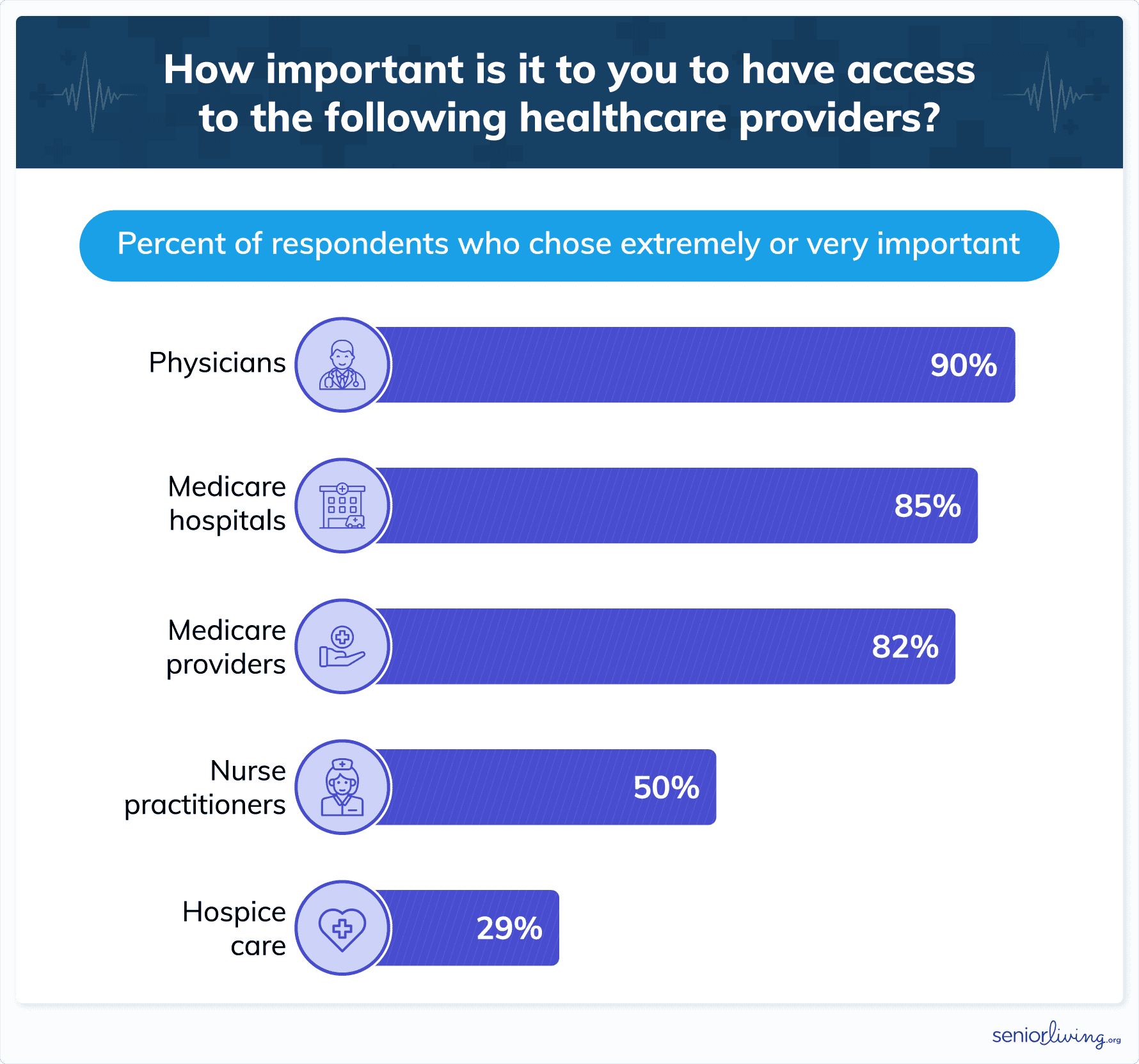
Older Americans are especially concerned about physician availability, and nearly as worried about accessing Medicare-certified providers and hospitals.
| States with best access scores | States with worst access scores |
|---|---|
| South Dakota | New Jersey |
| Montana | North Carolina |
| Mississippi | Georgia |
| West Virginia | Washington |
| North Dakota | New York |
Despite excellent accessibility in Mississippi and West Virginia, both states earned overall “F” grades because of their substandard medical costs and outcomes. We’ve seen that New York and New Jersey each feature excellent outcomes, but high population densities mean that provider-to-patient ratios are high.
Healthcare Costs for Seniors
As healthcare costs continue to rise, Medicare supplements grow pricier, and older Americans are forgoing medical treatment. Finding affordable healthcare is a paramount concern for seniors on fixed incomes. To measure the relative healthcare costs, we considered each state's average annual drug costs, insurance premiums, and out-of-pocket medical expenses (as a percentage of household income). Our research found that these expenditures proved equally important to Americans aged 65+.
Washington State has the best overall cost scores for prescription drugs and insurance premiums, while West Virginia had the worst.
| States with best cost scores | States with worst cost scores |
|---|---|
| Washington | West Virginia |
| Minnesota | New York |
| New Hampshire | Connecticut |
| Maryland | Wyoming |
| Virginia | Alabama |
Conclusion
Older Americans must weigh many factors when choosing where to spend their retirement years. Weather, cost of living, family proximity, crime rates, and leisure activities are all essential elements. Still, healthcare remains one of the most crucial considerations.
This issue is significant enough that two-thirds of Americans 65 or older report that candidates’ healthcare policies will be “very” or “extremely” important when casting their ballots this November.
Choosing a presidential candidate with a preferable policy isn’t the only way to improve one’s situation. Caregiving infrastructures vary widely from state to state, so older Americans can further help themselves by selecting the right place to live. The quality, affordability, and availability of medical care varies widely from state to state. One’s particular conditions and financial resources can significantly influence the selection of an optimal residential location.
SeniorLiving.org is proud to have sifted through a complex array of national data and determined the best and worst locales according to diverse criteria. Armed with this information, individuals can make the best choices for their particular situation and make the most of their golden years.
Our Data
The final score for each state was calculated by averaging the scores of three distinct categories which were weighted equally: costs, access, and outcomes. Each of those sub-score categories was determined by a state’s performance on a collection of metrics.
For each metric, states were given a score that represents their performance relative to all other states. The state with the best performance was given a score of 100 and the state with the worst performance was given a 0. All other states were then scored linearly on that scale. Scores were inverted for metrics where a lower value is preferred.
To ensure that the metrics were combined in a way that is most representative of the opinions of the senior population, we conducted a survey of 500 people aged 65+ to get their opinions on the importance of each metric. Respondents were asked to rate each metric for importance on a 5-point scale from not at all important to extremely important. Weights were determined based on the percentage of respondents who rated each metric as either very or extremely important. Finally, the sub-scores were calculated by calculating the weighted average.
The sources and metrics for each sub-category and their respective weights are as follows:
Cost:
An equal percentage of respondents rated all three metrics as either very or extremely important, so these were all weighted equally:
- Drug costs (33%)
- Out-of-pocket costs (33%)
- Average premiums (33%)
Access:
- Physicians per capita (27%)
- Hospices per capita (9%)
- Nurse practitioners per capita (15%)
- Medicare providers per capita (24%)
- Medicare hospitals per capita (25%)
Outcomes:
- Cancer mortality (27%)
- Stroke mortality (24%)
- Heart disease mortality (29%)
- Fall mortality (20%)
Data appendix
| State | Overall Rank (1 = best, 51 = worst) | Total adjusted score (50=lowest, 100=highest) | Unadjusted score | Cost score | Access score | Outcomes score |
|---|---|---|---|---|---|---|
| Alabama | 50 | 53.7 | 37.5 | 47.9 | 25 | 39.5 |
| Alaska | 16 | 83.3 | 55.1 | 71.2 | 26 | 68 |
| Arizona | 13 | 86.2 | 56.8 | 72.8 | 25.3 | 72.4 |
| Arkansas | 44 | 62.0 | 42.4 | 53 | 37.2 | 37 |
| California | 5 | 92.3 | 60.4 | 76 | 28.2 | 76.9 |
| Colorado | 15 | 85.7 | 56.5 | 75.6 | 19.7 | 74.3 |
| Connecticut | 38 | 68.7 | 46.4 | 39.6 | 20.1 | 79.4 |
| Delaware | 49 | 56.4 | 39.1 | 51 | 19.4 | 46.8 |
| District of Columbia | 30 | 73.7 | 49.4 | 49.6 | 42.3 | 56.2 |
| Florida | 39 | 68.5 | 46.3 | 56.1 | 18 | 64.7 |
| Georgia | 40 | 66.0 | 44.8 | 65 | 14.3 | 55.1 |
| Hawaii | 22 | 77.9 | 51.9 | 56.9 | 15.8 | 83.1 |
| Idaho | 11 | 87.5 | 57.6 | 77.1 | 29.7 | 65.9 |
| Illinois | 25 | 76.9 | 51.3 | 71.2 | 21.5 | 61.2 |
| Indiana | 31 | 73.2 | 49.1 | 72.1 | 25.3 | 49.8 |
| Iowa | 8 | 90.1 | 59.1 | 79.6 | 37.5 | 60.1 |
| Kansas | 6 | 91.6 | 60 | 77.6 | 45.3 | 57 |
| Kentucky | 42 | 63.6 | 43.4 | 60.3 | 32.8 | 37.1 |
| Louisiana | 41 | 65.7 | 44.6 | 54.2 | 43.5 | 36.1 |
| Maine | 27 | 75.8 | 50.6 | 60.8 | 33.9 | 57.2 |
| Maryland | 17 | 80.8 | 53.6 | 80.2 | 18 | 62.5 |
| Massachusetts | 9 | 89.4 | 58.7 | 69.2 | 24.8 | 82.2 |
| Michigan | 37 | 69.4 | 46.8 | 71.5 | 25.9 | 43.1 |
| Minnesota | 4 | 92.6 | 60.6 | 88.8 | 23.4 | 69.6 |
| Mississippi | 46 | 59.4 | 40.9 | 55.2 | 48.9 | 18.6 |
| Missouri | 32 | 72.1 | 48.4 | 64.2 | 33.5 | 47.6 |
| Montana | 1 | 100.0 | 65 | 79 | 49.6 | 66.3 |
| Nebraska | 12 | 86.7 | 57.1 | 58.3 | 43.2 | 69.7 |
| Nevada | 24 | 77.6 | 51.7 | 74.1 | 24.5 | 56.4 |
| New Hampshire | 7 | 91.6 | 60 | 83.3 | 27.1 | 69.7 |
| New Jersey | 20 | 78.5 | 52.2 | 58.9 | 12.3 | 85.5 |
| New Mexico | 10 | 89.4 | 58.7 | 76.2 | 30.3 | 69.6 |
| New York | 36 | 69.7 | 47 | 38.8 | 15 | 87.1 |
| North Carolina | 47 | 58.9 | 40.6 | 57.8 | 13.5 | 50.4 |
| North Dakota | 2 | 98.3 | 64 | 72.3 | 46.1 | 73.5 |
| Ohio | 35 | 71.4 | 48 | 72.1 | 28.6 | 43.4 |
| Oklahoma | 48 | 58.8 | 40.5 | 62.6 | 36.8 | 22.2 |
| Oregon | 28 | 75.3 | 50.3 | 78.9 | 19.5 | 52.4 |
| Pennsylvania | 29 | 75.1 | 50.2 | 70.1 | 22.8 | 57.7 |
| Rhode Island | 21 | 78.1 | 52 | 70.1 | 16.9 | 69.1 |
| South Carolina | 43 | 63.0 | 43 | 56.6 | 22.5 | 50 |
| South Dakota | 3 | 92.9 | 60.8 | 71.8 | 51.8 | 58.9 |
| Tennessee | 45 | 60.6 | 41.6 | 60.2 | 29 | 35.5 |
| Texas | 26 | 76.3 | 50.9 | 62.7 | 29.3 | 60.8 |
| Utah | 19 | 78.6 | 52.3 | 64.2 | 19 | 73.8 |
| Vermont | 33 | 71.7 | 48.2 | 50.5 | 33.2 | 61 |
| Virginia | 23 | 77.9 | 51.9 | 79.8 | 15.2 | 60.8 |
| Washington | 14 | 86.2 | 56.8 | 90.7 | 14.8 | 64.8 |
| West Virginia | 51 | 50.0 | 35.3 | 30.7 | 48.1 | 27.1 |
| Wisconsin | 34 | 71.5 | 48.1 | 72.6 | 21.4 | 50.3 |
| Wyoming | 18 | 80.5 | 53.4 | 43.3 | 45 | 71.8 |

